What is normal puberty?
Puberty occurs when your body undergoes physical changes from being a child to an adult.
Puberty occurs over a number of years:
- Between the age of 8 and 13 years (average of 11 years) in girls.
- Between 9-14 years (average of 11.5 years) in boys.
Girls start puberty with breasts development. Other changes include pubic hair growth, growth spurt, and finally periodic bleed (menstruation). Menstruation should occur before the age of 16.
Boys start puberty with testicular enlargement. However this early sign of puberty is often unnoticed. After the initial testicular enlargement, they will start growing pubic and facial hair, followed by growth spurt. The testicles and penis will continue to grow larger while the body will become more muscular.
Pubic hair growth which occur without other changes of puberty can be secondary to adrenarche (androgen hormones production from the adrenal glands) and thus may not be a sign of true pubertal onset.
What is delayed puberty?
Delayed puberty is defined as lack of:
- Breast development by age 13 years in girls.
- Testicular enlargement by age 14 years in boys.
What are the causes of delayed puberty?
These include:
- Constitutional delay in growth and puberty (CDGP).
This is the commonest cause of delayed puberty. However, other possible causes needs to be excluded before CGDP is diagnosed. - Underlying chronic illness.
- Children with uncontrolled diabetes, cystic fibrosis, kidney disease, heart and lung disease.
- Some medication such as high-dose steroid can cause stunted growth and delayed puberty.
- Teens with eating disorder (anorexia nervosa) who often lose too much weight.
- Girls who are extremely active in sports and are too lean. (Girls require a certain amount of body fat before they can enter puberty).
- Hypogonadism, due to a defect in the brain (hypothalamus/pituitary) or gonads (hypogonadism).
- Chemotherapy or radiotherapy.
- Certain genetic conditions interfering with normal growth processes:
- Turner syndrome (one of a female’s two X chromosomes is abnormal or missing).
- Klinefelter syndrome (boys born with an extra X chromosome, XXY instead of XY).
What is constitutional delay in growth and puberty (CDGP)?
Teens with CGDP is considered as the late bloomers.
- It is a normal variant of growth and development. Therefore, it is common to have another affected family member, such as parent, uncle, auntie, brothers, sisters, or cousins. The risk of having CGDP is higher if one or both parents were “late-bloomers”.
- CGDP is about twice as common in boys than girls.
- Among boys, about 60 % of delayed puberty is caused by CGDP.
How to approach teenagers with delayed puberty?
If a child is not developing puberty appropriately, medical consultation should be done.
The doctor will take detail medical history and perform necessary physical examination. Blood tests or radiograph may be ordered if indicated.
If no underlying disorder is detected, the doctor will reassure you that this is likely CGDP.
Puberty will eventually occur, but just slower than the peers.
When necessary, the child may be referred to a Paediatric Endocrinologist (doctor specialized in hormonal disorders in children) or to another specialist for further management.
When to refer to Paediatric Endocrinologist ?
Teenagers with delayed puberty should be referred to a Paediatric Endocrinologist when:
- The patient/parents feel anxious about the lack of pubertal development despite reassurance by the primary doctor.
- Evaluation of the gonadal axis is deemed necessary when hypogonadism is suspected.
- Pubertal induction with hormonal therapy is likely to be needed.
Does further investigations/tests indicated for teens with delayed puberty?
Majority of boys and girls with delayed puberty have CDGP which do not need detailed investigation.
Some of the investigations below may be done:
- Blood investigations for chronic disease such as full blood counts, renal function tests, urinalysis and inflammatory markers.
- Radiograph of the left wrist and hand to determine bone age, which is often delayed compare to the real age.
- Investigations related to disorders of gonadal axis may include the following:
- Chromosomes study (e.g. for Turner syndrome).
- Baseline hormones (follicle-stimulating hormone and luteinizing hormone, oestradiol or testosterone).
- Pelvic ultrasound in girls.
- Hormonal stimulation test (eg. GnRH test).
- MRI or CT scan of the pituitary and surrounding structures may be indicated in certain cases.
Due to the fact that there is no single test that can clearly differentiate CGDP from some other causes of hypogonadism, teenagers with CGDP must be followed up closely. Eventually normal pubertal development/progression will confirm the diagnosis of CGDP.
Treatment of delayed puberty
Treatment of delayed puberty will depend on the cause. Hormonal therapy for pubertal induction should ideally be under the guidance of a Paediatric Endocrinologist.
- For constitutional delay in growth and puberty (CDGP):
Hormonal treatment is usually not necessary. Instead, reassurance should be given and ensure appropriate monitoring. Puberty will eventually develop normally and normal final adult height is attained.
Though CGDP is a normal variant of growth, it may still make a child feel depressed under significant psychosocial and emotional stress. A short course of hormonal treatment may be offered to initiate puberty. After 4-6 months, the treatment is stopped, and the teenager’s body will take over to complete the process of puberty. - For underlying chronic disease:
Treat the underlying chronic disease; induction of puberty with hormone may be required in some patients. - For primary testicular and ovarian failure:
Pubertal induction with sex hormone followed by on-going lifelong hormone replacement. Increment of dosages should be gradual to prevent premature closure of the growth plate and thus cessation of growth.
Boys: Regular testosterone injections are available and are preferred.
Girls: Oral estrogen replacement is available. Cyclical progesterone therapy is added once maximal estrogen has been given or if breakthrough bleeding occurs. After that, a low-dose combined oral contraceptive pill can be used.
Counselling with respect to sexual function and fertility will be given as appropriate.
If these teenagers are depressed or having other problems related to delays in their growth and development, psychological counseling/therapy and medical consultation will be beneficial. This will help the teenager to adjust and cope with the situation in a positive way.
Tips for parents and teens:
Although delayed puberty is not harmful, it should not be overlooked. There are medical causes that need to be ruled out, although most of the time it is not due to underlying disease process.
Teenagers with delayed puberty need support as they may be teased at school and not accepted by their peers. They may feel as though they are never going to catch-up despite reassurance by the doctor.
Generally, pubertal delay by itself does not affect fertility. However, certain medical conditions causing hypogonadism can affect fertility.
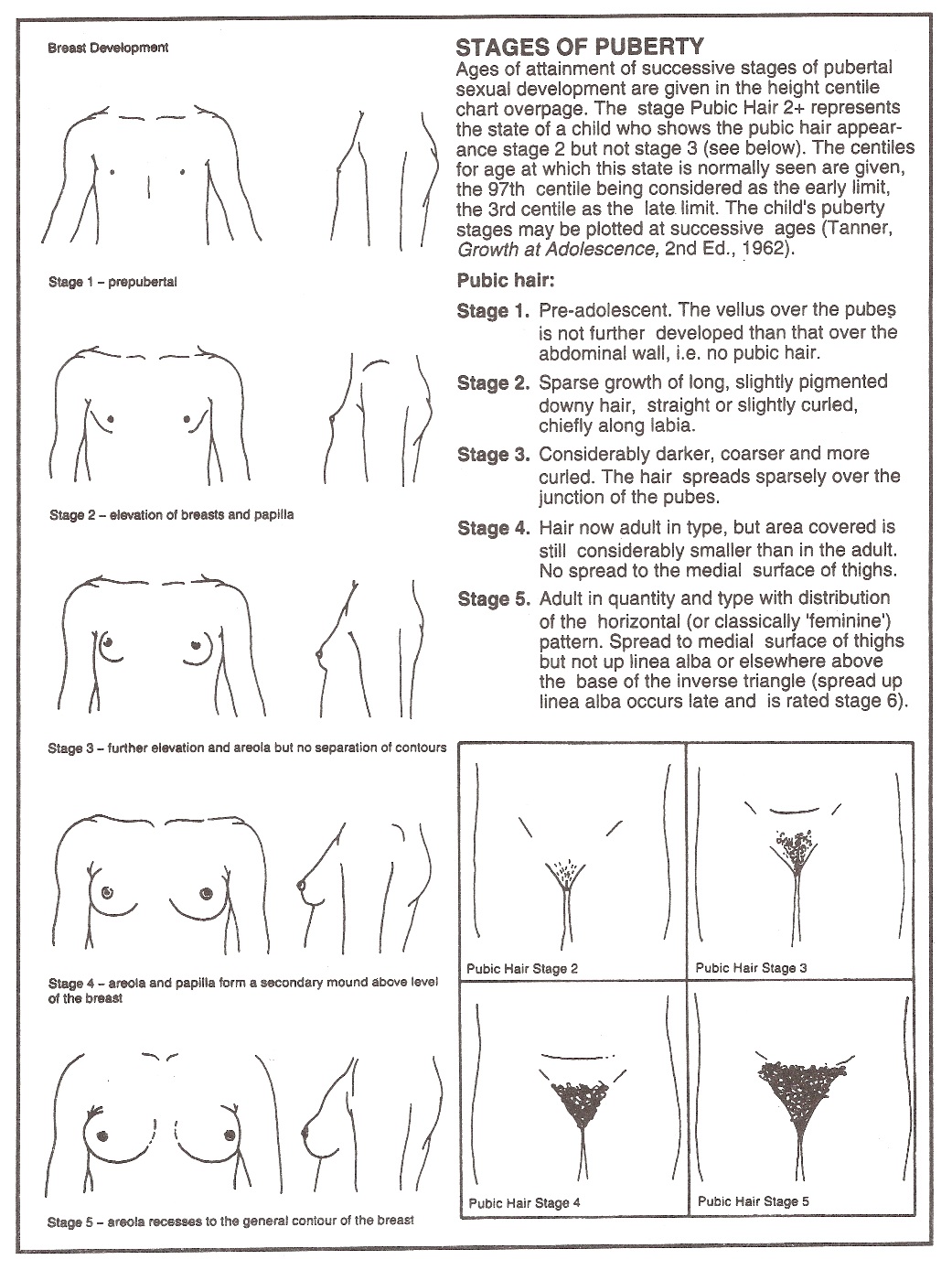 |
| Picture 1: Stages of pubertal progression in girls |
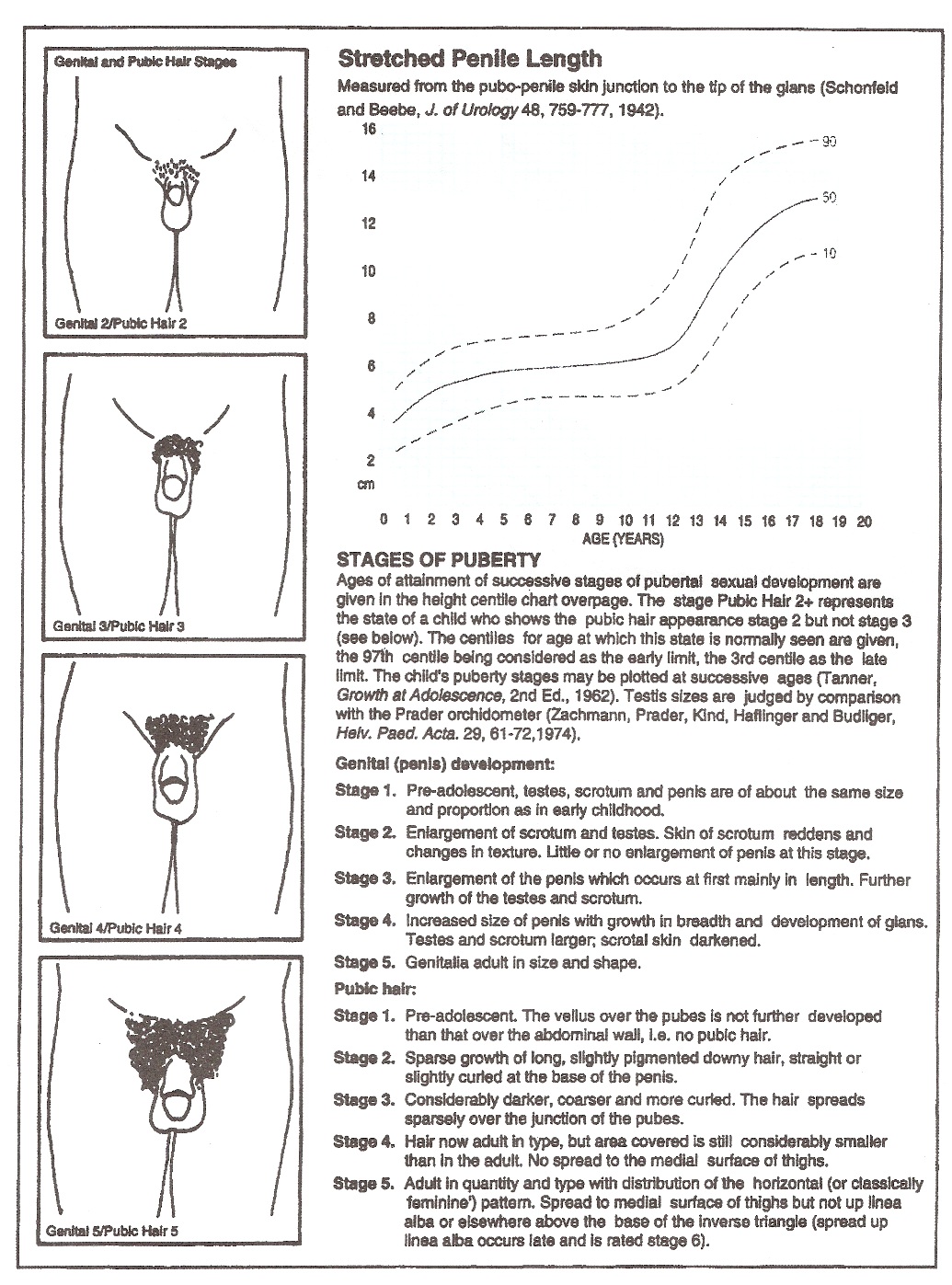 |
| Picture 2. Stages of pubertal progression in boys |
Reference :
- Madhusmita Misra, Mary M Lee; Delayed Puberty. Paediatric Endocrinology, The Requisites in Pediatrics, Chapter 6, 1st edition, 2005.
- Bramswig J, Dubbers A; Disorders of pubertal development. Dtsch Arztebl Int. 2009 Apr;106(17):295-303; quiz 304. Epub 2009 Apr 24.
- Clark PA; Constitutional Growth Delay, Medscape, Aug 2009.
- Ambler GR; Androgen therapy for delayed male puberty. Curr Opin Endocrinol Diabetes Obes. 2009 Jun;16(3):232-9.
| Last Reviewed | : | 28 August 2020 |
| Writer | : | Dr Janet Hong Yeow Hua |
| Reviewer | : | Dr. Zainab bt. Kusiar |







